Clinical Pharmacy Integration Part 2
So what is ‘Clinical Pharmacy Integration’? At its most basic, it might involve initiatives to improve coordination around a single disease, typically asthma or diabetes. At its most sophisticated, it might encompass fully integrated hospital systems with closed staffs consisting entirely of employed physicians. Most hospitals and health systems are somewhere in-between.
When 82-year-old Jack Schlichting was admitted to the Henry Ford Hospital in Detroit five years ago with a badly broken leg, he received standard hospital treatment: initial care in the trauma center, surgery and some time in the hospital recovering. But his discharge from the hospital did not mark the end of Schlichting’s care by the Henry Ford Health System, a large, diverse health care organization that is an established leader in clinical integration.
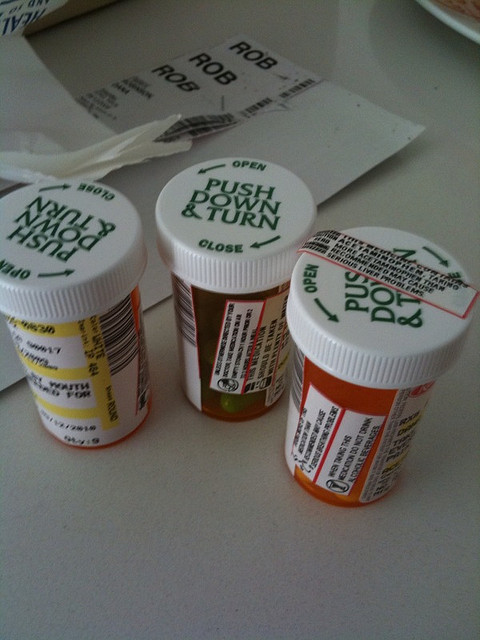
While Schlichting recovered at his daughter’s house, under the care of the Henry Ford home health care program, he went through extensive rehabilitation at another of the system’s hospitals. All the while, his care was supervised by physicians of the Henry Ford Medical Group. He found a wheelchair through Henry Ford’s durable-medical-equipment company and ordered his medication from the system’s pharmacies.
And while this explanation focuses primarily on the ‘coordination’ of care, I believe that true integration, in order to be successful, relies on one final piece – the thoughtful application of domain experts with technology solutions in a coordinated manner.
In other words, identifying the weaknesses in our workflow and creating mechanisms to apply solutions by the folks that are considered ‘experts’ in the domain, supportive IT platforms to aid in their efficiency.
Basically, get the folks that love that particular task hardwired into the workflow for that task.
Consider our current workflow for medicine reconciliation in the ED. The ED physician does a cursory med reconciliation during his all-important initial H&P, gathering information towards a working diagnosis and management plan. Upon the decision to admit, the ED nurse is charged with the task of completing a comprehensive medicine reconciliation prior to the admitting internist or family practitioner seeing the patient.
The hard truth of the matter is that accurate medicine reconciliation is one of the most labor intensive processes that this nurse will face in his / her shift, under the guise of a simple list of medications. Aside from the accuracy of the list itself, there are myriad other considerations:
-
Accuracy of the medication dosage, schedule, frequency.
-
Accuracy of whether the patient is in fact taking the medication
-
Accuracy of whether this list coincides with the most recent prescribed medication list from the PCP and/or the pharmacy
-
The investigative work required to accurately identify medications described from memory by the patient, ie ‘That Little Purple Pill’
The simple truth is that a medicine reconciliation approaching 100% accuracy can take as much as 30 minutes of concentrated effort with calls being made to family, pharmacies and PCP offices taking up the bulk of that time.